Impact of sex and gender aspects in depression/Introduction
Contents
Incidence/Prevalence
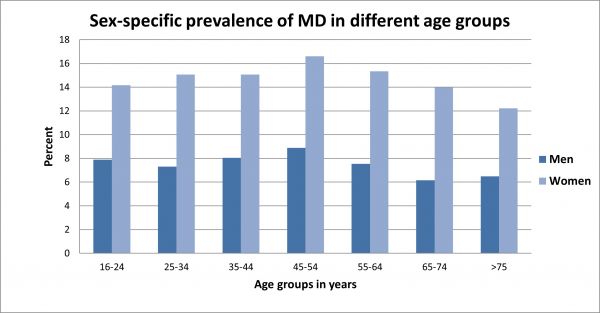
Epidemiological studies show that women suffer from depression significantly more often than men. Longitudinal studies, which allow an estimation of the incidence rates of depressive disorders within a particular time frame, find consistently higher rates of new cases in girls and women (a period of 12 to 20 months showed incidences between 1.6 and 3.4 percent) compared to boys and men. [1] [2] According to data collected in a study evaluating the health of adults in Germany, 13.1 percent of women and 6.4 percent of men aged 18 to 64 years were suffering from depression in 2014 (12-month prevalence). [3] Therefore, women are presumed to suffer from depressive symptoms about twice as often as men. The so-called "gender gap" is especially noticeable with seasonal and atypical depression. [4] [5] [6] In general, differences in prevalence between the sexes have been shown to be internationally consistent. Less clear however, are the conclusions regarding differences in the clinical course of depression in men and women. Nevertheless, the majority of studies show higher relapse and chronification rates in women than in men. [7]
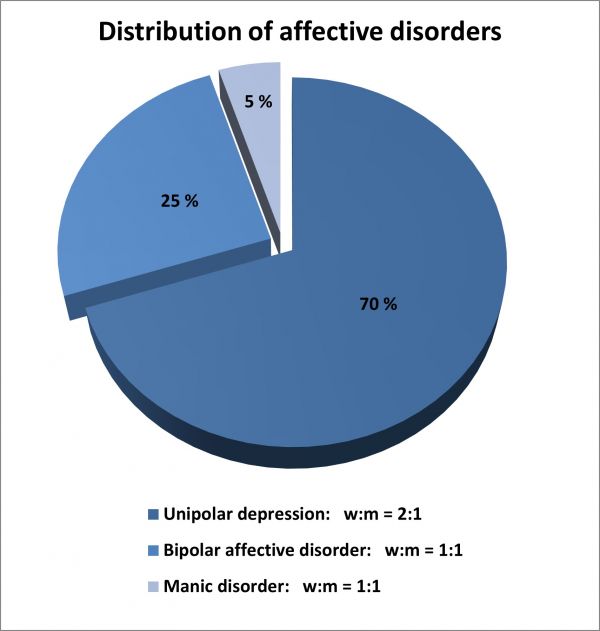
Figure 1: Distribution of affective disorders and sex ratio (female: male) [Source: GenderMed-Wiki]
In contrast to unipolar depression, bipolar disorders and manic disorders do not appear to demonstrate any sex difference in prevalence rates; women and men seem to be affected equally. A general sex-specific difference in the prevalence of affective disorders can therefore not be assumed (see Figure 1). Nevertheless, the course and exact symptoms of bipolar disorders vary between the sexes. [7]
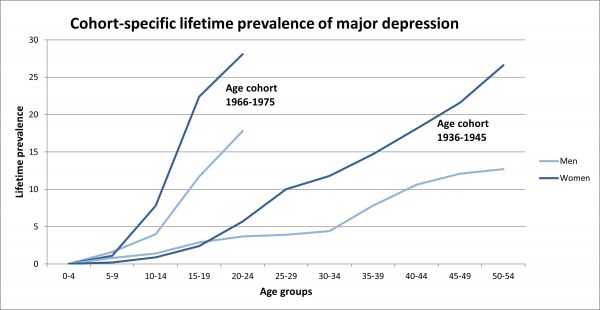
Figure 2: Cohort-specific lifetime prevalence of major depression in women and men [Source: GenderMed-Wiki, by Kessler et al., 1994].
Figure 3: Sex-specific differences in the prevalence of major depression in different age cohorts (6-month prevalence) [Source: GenderMed Wiki, according to Angst et al., 2002].
Research on the age-related sex difference shows that the depression rate between female and male patients only really begins to differ at the onset of puberty. [8] During puberty, the prevalence increases overall, with a much greater increase in girls. By the age of 18, women are already twice as likely to suffer from depression as men. [2] It is currently unclear whether the prevalence figures of both sexes converge again in late adulthood. [9]
Risk and protective factors
Studies overwhelmingly confirm the female sex as a risk factor for the development of a depressive episode. The following table lists important biological and psychosocial predictors that are scientifically investigated as causes of this sex difference (Table 1). Psychosocial factors influencing both sexes can be found in section 4.4 ('Psychosocial factors').
Table 1: Biological and psychosocial factors in comparison.
| Biological factors |
Psychosocial factors |
|
Genetic risk: Recent studies indicate a stronger genetic predisposition in women compared to men (heritability for women between 40 to 42 percent and for men 29 to 31 percent). [10] In addition, there are indications that some genetic risk factors may have different effects on women than men or only be relevant to one sex. [11] |
Primary anxiety disorder: It is estimated that the presence of primary anxiety disorder explains about 50 percent of the association between sex and the prevalence of depression: epidemiological studies show that the diagnosis of an anxiety disorder significantly increases the risk of developing depression in both men and women. However, women are affected by anxiety disorder significantly more often than men, which give this risk factor a sex-specific orientation. [12] |
|
Phases of hormonal change: 1. Puberty: Pubertal maturation is a good predictor of adolescent depression in girls. [13] Under certain circumstances, the increase in sex hormones may be directly related to the development of negative affect in girls. [14] Pubertal status should not be considered an isolated biological factor; rather there exists a complex interaction with social and cultural variables (e.g. the search for identity). [9] 2. Premenstrual dysphoric syndrome (PMDS): An increased sensitivity to changes in estrogen and progesterone levels is believed to have a negative effect on serotonin metabolism. However, reliable measurement of central nervous serotonin functionality is not yet possible. [9] It is suggested that PMDS be regarded as an independent disorder, as it differs from a depressive episode in its primary symptoms (irritability, affect lability), phase duration and drug latency (SSRI). [15] 3. Postpartum phase: Postpartum depression is defined as a major depression that begins within four weeks of giving birth. While up to 70 percent of women develop individual depressive symptoms after childbirth, about 13 percent appear to suffer from a depressive episode during this period. Studies show that in the first three to four days after giving birth, the estrogen level drops dramatically. In proportion to this loss of estrogen, the level of the enzyme monoaminooxidase A (MAO-A) in the female brain seems to increase significantly. This enzyme is found in higher concentrations in glial cells and monoamine-releasing neurons, where it reduces the availability of the neurotransmitters serotonin, dopamine and norepinephrine. Among other things, these neurotransmitters have an impact on mood. If these neurotransmitters are deficient, there may initially be feelings of sadness, but later an increased risk of developing depression. [16] Predictors such as depressive illness in the medical history and/or during pregnancy, lack of social support and stressful life events were also identified. [17] In some cases, men can also develop postpartum depression, although the prevalence here is significantly lower (4 to 5 percent). [18] 4. (Peri-)Menopause: Several studies confirm an increased risk of relapse in women with earlier depressive episodes [19] and an increase in depressive symptoms in women who are not already depressed [20] during perimenopause. It remains unclear whether hormonal changes have a direct influence or indirectly modulate the relationship via vasomotor symptoms and/or critical life events. [9] The effectiveness of estrogen replacement therapies for depressive symptoms remains inconsistent. [21] |
Personality traits: Sex differences in personality related vulnerability factors are particularly evident in late adolescence and young adulthood: For example, lower self-esteem [22] and higher neuroticism [23] seem to increase the risk of depression in girls and women in these phases of life. In addition, girls show significantly higher anxiety scores than boys even before the onset of puberty (and thus before depression rates drift apart between the sexes). [22] A prominent cognitive approach to gender differences in depression is the ''Response Styles Theory'', which deals with coping strategies in managing depressive disorders. Emotionally focused, symptom-related worrying (rumination) can result in an exacerbation of depressive symptoms. In most cases, feelings of rumination are much more pronounced in women than in men. In comparison, men are more likely to cope through cognitive and behavioral distraction, which frequently has depression-reducing effects. These different coping styles are mainly due to gender-specific socialization processes. [24] |
|
Neuroendocrine stress response: There is a hypothesis being discussed that sex hormones modulate a greater dysregulation of the HPA axis in women. [25] However, studies show that women with low estrogen production (luteal phase) respond to psychological stress with a similar cortisol release as men. With high estrogen production (follicular phase or taking contraceptives) women respond with a lower cortisol release than men. [26] |
Psychosocial stressors: Women are particularly vulnerable to psychosocial stressors in the macro-social sphere: Factors such as low levels of education, low socio-economic status (even poverty) or low control over behavior are structural aspects that have a negative impact on the mental health of women and men. However, it is usually women who are significantly disadvantaged with regard to these factors. [27] Life-event research also confirms that although women and men tend to have a similar risk of responding to stressful life events with depression, women are subjected to significantly more negative events affecting their social environment than men. [10]</ref> Even in adolescence, girls experience interpersonal stress more often, to which they respond with depression. [28] |
|
Oxytocin: High interpersonal needs and the desire for intimacy in women are regulated in part by the sex hormone oxytocin. Women in particular are vulnerable to the development of depression with regard to interpersonal stress. Risk factors here are an unstable parental attachment, an anxious, repressive nature and low instrumental coping strategies (e.g. rumination). [29] Sufficient empirical results from human research are not yet available. |
Sexual and non-sexual physical violence: Sexual and non-sexual physical violence are traumatic stressors that can lead to the development of various mental illnesses. [30] In these cases, men and women become victims of violence. While men are exposed to physical violence in public places much more often, women are significantly more prone to severe forms of domestic and sexual violence. According to data from the BMFSFJ from 2004, approximately 13% of women in partnerships are exposed to domestic violence. [31] The consequences of this violence may not only be psychological and physical injuries, but also chronic pathological changes in the HPA axis. [32] |
Symptoms
While women tend to show core symptoms such as sadness, in men these can be masked by external symptoms such as aggressiveness. [Source: GenderMed Wiki, 2016]
While depressive core symptoms such as sadness, depression and anhedonia are mentioned by both sexes with about the same frequency, other depressive symptoms can differ between the sexes. [33] For this reason, depression in men often goes unrecognized. Researchers speak of "depression blindness" in men, which seems to have various causes. One important aspect is that depression symptoms sometimes manifest themselves differently in men than in women. For example, men tend to react aggressively and take risks during a depressive episode and resort to alcohol and drugs more often than women. These external signs often mask the "classic" clinical symptoms, such as loss of self-esteem, listlessness or loss of pleasure, especially at the onset. [34] Such behavioral patterns are often not recognized by professionals as possible depression symptoms but are classified as "typical male defense strategies". [35] In contrast, women are more likely than men to react with atypical symptoms (e.g., increased appetite instead of loss of appetite) or somatic complaints and pain. [33] Overall, they report more symptoms than their male counterparts. [5]
Although the prevalence of depression is significantly higher among women, men are three times more likely to commit suicide than women (with women more likely to make an attempt). Women tend to be more parasuicidal, while men tend to use more aggressive methods. Up to 70 percent of all suicides occur in the context of a depressive illness. [36]
The increased suicide rate accompanied by a lower rate of attempted suicide in the male population compared to the female population is scientifically discussed as a so-called ''gender paradox'' and allows the hypothesis that the low depression prevalence in men is due less to a lower risk of depression than to underdiagnosis (detailed information on gender differences in suicide and suicidal behavior can be found here). [37] [38]
Concerning the clinical picture of men with depression, the following can be observed: The stronger the adherence to stereotypical ideals of masculinity (normative or hegemonic masculinity), the more pronounced the externalized symptoms of depression [39] and the more probable a suicide attempt. [40] In order to be able to reduce suicide rates in men, a male pattern of symptoms must be taken into account in diagnosis and therapy. [41]
The following table (Table 3) illustrates the distribution of depressive symptoms between the sexes. No clear differences between sexes can be assumed here; only trends and results of individual studies are shown.
Table 3: Potential Differences in the manifestation of symptoms between men and women.
| Women > Men | Men > Women |
| Physical symptoms: energy loss, fatigue, sleep disorders, appetite disorders, motor and cognitive retardation [42] [6] | Emotional arousal: aggressiveness, anger, [43] fits of anger and irritability [35] |
| Atypical symptoms: Weight gain, increased appetite, increased sleep. [5] | Substance abuse/dependence: alcohol, nicotine, drugs [34] |
| Other: Comorbid anxiety with nervousness and/or panic attacks [5], physical complaints and pain [42] | Social interaction: hostility, uncontrolled actions, tendency to reproach outwardly, antisocial behavior. [35] [34] |
Prevention
Effective coping strategies for mental stress can prove to be successful in preventing the development of a depressive episode. Coping does not have positive (in the sense of health-promoting) effects per se, but rather "wrong" strategies can promote the development of depressive symptoms or aggravate existing complaints. It is therefore necessary to differentiate between health-promoting and health-damaging coping in the prevention and treatment of depressive disorders. Studies confirm sex and gender differences exist in dealing with stressful situations on a cognitive and behavioral level. Overall, women seem to cope with stress in a more emotionally centered way, tend to brood more easily and are less able to distance themselves. Men are better able to distract themselves but tend to react with emotional inhibition in problem situations and are significantly less likely to seek professional help. [44] [5] The following overview (Table 4) presents research results on gender-specific coping behavior in table form.
Table 4: Gender differences in coping behavior.
| Women > Men | Men > Women |
| Women seem to cope more emotionally focused and use emotions as a "valve" (e.g. by crying, shouting or even laughing) In addition, they more often state that they find relief in their (religious) beliefs. [24] | Men cope more often in an action-oriented way, for example by becoming more active in sports (positive) or increasing their alcohol consumption (negative, risk of comorbid addiction). [24] |
| Women tend to cope in an emotionally focused and symptom-related way and have a stronger tendency to brood with thought processes (rumination). Rumination enhances the risk of exacerbation of depressive symptoms. [5] | Men are more likely to cope with cognitive and behavioral distraction, which prevents rumination and can reduce symptoms. [5] |
| Women tend to have an emotionally focused and avoiding coping style, cope less rationally and are less able to distance themselves. [44] | Men react more emotionally blocked in difficult situations than women. [44] |
| Men are much less likely than women to seek professional support for psychological problems. [45] |
External Links
- Neurologen und Psychiater im Netz (2013). Reizbarkeit, Ärger, Sucht sind typische Depressionssymptome bei Männern.
- Möller-Leimkühler, A. M. (2012). Depression bei Männern: Eine Einführung. Journal für Neurologie, Neurochirurgie und Psychiatrie, 11(3), 11-20.
Literature
- Bijl RV, Graaf R de, Ravelli A, Smit F, Vollebergh WAM. Gender and age-specific first incidence of DSM-III-R psychiatric disorders in the general population. Soc Psychiatry Psychiatr Epidemiol 2002; 37(8):372–9.
- Oldehinkel, A. J., Wittchen, H. U., & Schuster, P..Prevalence, 20-month incidence and outcome of unipolar depressive disorders in a community sample of adolescents. Psychological Medicine 1999, 29(03), 655-668.
- Jacobi F, Höfler M, Siegert J, Mack S, Gerschler A, Scholl L et al. Twelve-month prevalence, comorbidity and correlates of mental disorders in Germany: The Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH). Int. J. Methods Psychiatr. Res. 2014; 23(3):304–19.
- Winkler D, Praschak-Rieder N, Willeit M, Lucht MJ, Hilger E, Konstantinidis A et al. Saisonal abhängige Depression in zwei deutschsprachigen Universitätszentren: Bonn, Wien Klinische und demographische Charakteristika. Nervenarzt 2002; 73(7):637–43.
- Angst J, Gamma A, Gastpar M, Lépine J, Mendlewicz J, Tylee A. Gender differences in depression. Epidemiological findings from the European DEPRES I and II studies. European archives of psychiatry and clinical neuroscience 2002; 252(5):201–9.
- Marcus SM, Young EA, Kerber KB, Kornstein S, Farabaugh AH, Mitchell J et al. Gender differences in depression: Findings from the STAR*D study. Journal of Affective Disorders 2005; 87(2-3):141–50.
- Kuehner C. Gender differences in unipolar depression. Acta Psychiatrica Scandinavica 2003; 108(3):163–74.
- Essau CA, Petermann U. Depression bei Kindern und Jugendlichen. Zeitschrift für klinische Psychologie, Psychopathologie; 43:18–33.
- Kühner C. Warum leiden mehr Frauen unter Depressionen? In: Lautenbacher S, editor. Gehirn und Geschlecht: Neurowissenschaft des kleinen Unterschieds zwischen Frau und Mann. Heidelberg: Springer; 2007.
- Kendler KS, Gatz M, Gardner CO, Pedersen NL. A Swedish National Twin Study of Lifetime Major Depression. AJP 2006; 163(1):109–14.
- Sullivan PF, Neale MC, Kendler KS. Genetic Epidemiology of Major Depression: Review and Meta-Analysis. AJP 2000; 157(10):1552–62.
- Breslau N, Schultz L, Peterson E. Sex differences in depression: A role for preexisting anxiety. Psychiatry Research 1995; 58(1):1–12.
- Patton GC, Hibbert ME, Carlin J, Shao Q, Rosier M, Caust J et al. Menarche and the onset of depression and anxiety in Victoria, Australia. Journal of Epidemiology & Community Health 1996; 50(6):661–6.
- Angold A, Costello EJ, Erkanli A, Worthman CM. Pubertal changes in hormone levels and depression in girls. Psychological Medicine 1999; 29(5):1043–53.
- Landén M, Eriksson E. How does premenstrual dysphoric disorder relate to depression and anxiety disorders? Depress. Anxiety 2003; 17(3):122–9.
- J. Sacher, A. A. Wilson, S. Houle, P. Rusjan, S. Hassan, P. M. Bloomfield, D. E. Stewart, J. H. Meyer Elevated Brain Monoamine Oxidase A Binding in the Early Postpartum Period Archives of General Psychiatry 67(5):468-474 (2010).
- O'hara MW, Swain AM. Rates and risk of postpartum depression—a meta-analysis. International Review of Psychiatry 2009; 8(1):37–54.
- Ballard CG, Davis R, Cullen PC, Mohan RN, Dean C. Prevalence of postnatal psychiatric morbidity in mothers and fathers. The British Journal of Psychiatry 1994; 164(6):782–8.
- Harlow BL, Wise LA, Otto MW, Soares CN, Cohen LS. Depression and Its Influence on Reproductive Endocrine and Menstrual Cycle Markers Associated With Perimenopause. Arch Gen Psychiatry 2003; 60(1):29.
- Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of Hormones and Menopausal Status With Depressed Mood in Women With No History of Depression. Arch Gen Psychiatry 2006; 63(4):375.
- Amin Z. Effect of Estrogen-Serotonin Interactions on Mood and Cognition. Behavioral and Cognitive Neuroscience Reviews 2005; 4(1):43–58.
- Feingold A. Gender differences in personality: A meta-analysis. Psychological Bulletin 1994; 116(3):429–56.
- Costa, Paul, Jr., Terracciano A, McCrae RR. Gender differences in personality traits across cultures: Robust and surprising findings. Journal of Personality and Social Psychology 2001; 81(2):322–31.
- Nolen-Hoeksema S. The Response Styles Theory. In: Papageorgiou C, Wells A, editors. Rumination: Nature, theory & treatment for nagative thinking in depression. Chichester: Wiley; 2003.
- Young EA, Altemus M. Puberty, ovarian steroids, and stress. In: Dahl RE, Spear LP (eds) Adolescent brain development: Vulnerabilities and opportunities. New York Academy of Sciences, New York, 2004, pp 124–133.
- Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. Impact of gender, menstrual cycle phase, and oral contraceptives on the activity of the hypothalamus-pituitary-adrenal axis. Psychosomatic medicine 1999; 61(2):154–62.
- Belle Doucet DJ. Poverty, Inequality, And Discrimination As Sources Of Depression Among U.S. Women. Psychology of Women Quarterly 2003; 27(2):101–13.
- Shih JH, Eberhart NK, Hammen CL, Brennan PA. Differential Exposure and Reactivity to Interpersonal Stress Predict Sex Differences in Adolescent Depression. Journal of Clinical Child & Adolescent Psychology 2006; 35(1):103–15.
- Cyranowski JM, Frank E, Young E, Shear MK. Adolescent Onset of the Gender Difference in Lifetime Rates of Major Depression. Arch Gen Psychiatry 2000; 57(1):21.
- Campbell JC. Health consequences of intimate partner violence. The Lancet 2002; 359(9314):1331–6.
- Bundesministerium für Familie, Senioren, Frauen und Jugend. Lebenssituation, Sicherheit und Gesundheit von Frauen in Deutschland. Eine repräsentative Untersuchung zu Gewalt gegen Frauen in Deutschland. Baden-Baden: Bundesministerium für Familie, Senioren, Frauen und Jugend; 2004.
- Griffin MG, Resick PA, Yehuda R. Enhanced Cortisol Suppression Following Dexamethasone Administration in Domestic Violence Survivors. AJP 2005; 162(6):1192–9.
- Lautenbacher S. Gehirn und Geschlecht: Neurowissenschaft des kleinen Unterschieds zwischen Frau und Mann. Heidelberg: Springer; 2007.
- Weißbach L, Stiehler M. Männergesundheitsbericht 2013: Im Fokus: Psychische Gesundheit. Bern: Hans Huber; 2013.
- Möller-Leimkühler AM, Paulus, N-C, Heller J: Male Depression in einer Bevölkerungsstichprobe junger Männer: Risiko und Symptome. Der Nervenarzt, 2007, 78 (6): 641-650
- Gößwald A, Lange M, Kamtsiuris P, Kurth B. DEGS: Studie zur Gesundheit Erwachsener in Deutschland. Bundesgesundheitsbl. 2012; 55(6-7):775–80.
- Canetto SS, Sakinofsky I. The Gender Paradox in Suicide. Suicide and Life-Threatening Behavior 1998; 28(1):1–23.
- Möller-Leimkühler, A. M. (2012). DFP: Depression bei Männern: Eine Einführung. Journal für Neurologie, Neurochirurgie und Psychiatrie, 11(3), 11-20.
- Magovcevic M, Addis ME. The Masculine Depression Scale: development and psychometric evaluation. Psychol Men Masc 2008; 9: 117–32.
- Houle J, Mishara BL, Chagnon F. An empirical test of a mediation model of the impact of the traditional male gender role on suicidal behavior in men. J Affect Disord 2008; 107: 37–43.
- Rutz W (1999) Improvement of care for people suffering from depression: the need for comprehensive education. Int Clin Psychopharmacol 14: 27–33.
- Silverstein B. Gender Differences in the Prevalence of Somatic Versus Pure Depression: A Replication. AJP 2002; 159(6):1051–2.
- Neurologen und Psychiater im Netz. Das Informationsportal zur psychischen Gesundheit und Nervenerkrankungen. Reizbarkeit, Ärger, Sucht sind typische Depressionssymptome bei Männern; 2013.
- Matud PM. Personallity and Indvidual Differences. Personality and Inividual Differences 2004; 37(7).
- Addis ME, Mahalik JR. Men, masculinity, and the contexts of help-seeking. American Psychologist 2003; 58.
License
This article is published under the Creative Commons License. The full license content can be retrieved here: https://creativecommons.org/licenses/by/3.0/legalcode
Autoren
Paulina Juszczyk
Last changed: 2021-10-23 13:10:04